AUTOLOGOUS CHONDROCYTE IMPLANTATION - STEM CELLS IMPLANTATION
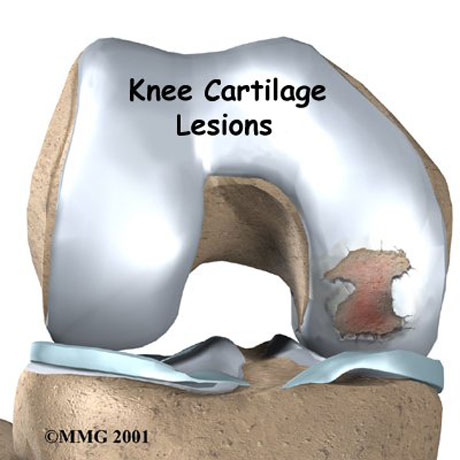
Injuries to joint surfaces can result from acute high-impact or repetitive shear and torsional loads to the superficial zone of the articular cartilage architecture. The use of autologous chondrocyte implantation is promising and is associated with several potential long-term benefit.
Autologous chondrocyte implantation is ideally suited for symptomatic deep chondral lesion along the femoral condyle or trochlear region. High-demand patient between 15-55 years of age with excellent motivation and potential for compliance are the best candidates.
However autologous chondrocyte implantation is a viable option for a symptomatic patient with a lesion of >2 sq.cm but <12 sq.cm. and for a patient who continues to have pain after mosaicplasty or microfracture procedure. Bone involvement is not contraindication, but staged or concomitant autologous bone grafting should be undertaken when the bone involvement is deeper than 6-8 mm.
Autologous chondrocyte transplantation is not a treatment for osteoarthritis (general joint disease), gout, and rheumatoid arthritis or other systemic joint diseases.
X-ray oft the left knee. Osteochondritis Dissecans of the left knee (medial femoral condyle)
MRI: Osteochondritis Dissecans of the knee.
Talus cartilage lesion
Cartilage fragment of the medial femoral condyle - Knee.
Autologous chondrocyte are arthroscopicaly harvested from a less weight-bearing area, commercially extracted from the harvested cartilage (200-500mg), and multiplied in vitro (labor cell culture).
Elective reinplantation is performed 4-6 weeks after cartilage harnesting by debridement of the defect to an intact margin, carelully avoiding osseous bleeding from the bed of the defect.
The lesion area is already clear and ready to receveive the autologous chondrocyte.
Cartilage cell culture in Bioengeneering Lab in Greece.
Chondrocyte culture.
The surgeon cut the chondrocyte film like the shape of the chondral defect.
The autologous chondrocyte is ready to implant.
The autologous chondrocyte is transplanted. The chondral defect is covered.
Chondral defect due to trauma.
The autologous chondlal cell filling the defect.
The chondral defect covered by autologous chondrocyte atrhoscopically.
The procedure is finished. The knee movement is without any problem.
REHABILITATION
Postoperatively protected weight-bearing are restricted for 6 weeks. The crutches is necessary for walking.
The physical therapy program started 2nd post-op day with passive movement (physical therapist or CPM machine) until 4th week.
Therapy concentrates on quadriceps activation and isometric straight leg raises. After the 6th week the patient can walk without aid devices with full weight-bearing. Full weight bearing and full range of motion are achieved. Closed-chain exercises and functional training are started.
After 12th week Strengthening and functional training are progressed. Return to full activities is delayed for at least 8 months to protect the lesion as it matures.
Return to participation in pivoting sports is usually allowed by 12 months.
ESSKA Congress, Geneva. Poster presentation, "Osteochondritis Dissecans of the knee. Chondrocyte implantation combine with corrective osteotomy"


