DISTAL BICEPS TENDON RUPTURE
Rupture of the distal biceps tendon is a relatively rare injury. The majority of ruptures occurs proximally; distal ruptures represents only 3% of all biceps tendon ruptures, with an incidence of 1.2 of 100.000 person per year.
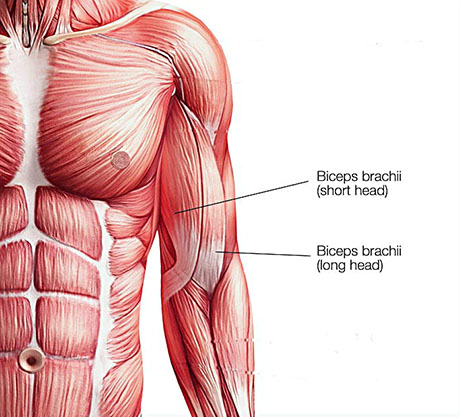
ANATOMY
The biceps has two tendons that attach the muscle to the bone in the shoulder and one tendon that attaches at the elbow. The tendon at the elbow is also called the distal biceps tendon. It attaches to the radial tuberosity. This is a small bump on one of the bones in your forearm (radius) near your elbow joint.
HISTORY AND PHYSICAL EXAMINATION
Patients with biceps tendon ruptures often present with a history of acute onset of pain in the front side of the elbow during lifting. The typical patient is a 50 years old but may be between 21 and 70 years of age; a majority of cases occur in weight lifters.
Smoking. Nicotine use can affect nutrition in the tendon.
Corticosteroid medications. Using corticosteroids has been linked to increased muscle and tendon weakness.
Patient report ecchymosis anterior to the elbow and a period of limited elbow motion secondary to acute inflammation and swelling in the region. If care is sought after the acute inflammation has , patient may present with complaints of weak elbow flexion and supination.
Distal biceps tendon rupture. The tendon is contracted proximally.
Distal biceps tendon rupture. The Orthopaedist index finger shows the gap produced by rupture.
Long head biceps tendon rupture in young man
DIAGNOSTIC IMAGINE
Radiograph are typically normal. On occasion avulsion of the tuberosity have been demonstrated in the acute setting.
If the physical examination is conclusive, further imaging is not required.
Magnetic resonance imaging (MRI), can help to confirm the diagnosis if the physical examination findings are unclear.
Ultrasonography has also been shown to be an inexpensive and reliable method to confirm diagnosis of biceps rupture, although this technique requires a skilled ultrasonographer for accurate interpretation.

Magnetic resonance imaging: Massive rupture of distal biceps tendon, Red circle ruptured biceps tendon contracted proximaly. Red arrow, the gap.


