INTERVERTEBRAL DISC HERNIATION
The lifetime incidence of low back pain ranges from 50-80%, whereas the incidence of sciatica ranges from 13-40%
INTERVERTEBRAL DISC ANATOMY
Intervertebral discs are found between each vertebra.
The human disc has two basic parts: an inner jell o-like center called the Nucleus Pulposus and the Annulus Fibrosis
The Nucleus Pulposus is the water-rich, gelatinous center of the disc. It has three main functions:
- to bear or carry the downward weight (i.e., axial load) of the human body
- act as a 'pivot point' from which all movement of the lower trunk occurs.
- act as a ligament and bind the vertebrae together.
Lumbar spine anatomy
The Annulus Fibrosus is much more fibrous (tougher) than the nucleus. It also has a much higher collagen content and lower water content when compared to the nucleus.
Its main job is hold in place or contain the highly pressurized nucleus (the nucleus is pressurized for hold up the weight of the body), which is constantly trying to escape its central prison.
The annulus is made of concentric sheets of collagen (a tough cartilage-like substance) that are called Lamellae. The lamellae are arranged in a special configuration that makes them extremely strong and assists in their job of containing that pressurized nucleus pulposus.
WHAT IS DISC HERNIATION?
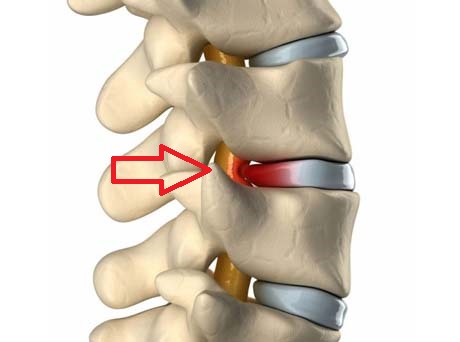
Disc herniation occurs when the annulus fibrous breaks open or cracks, allowing the nucleus pulposus to escape. This is called a Herniated Nucleus Pulposus (HNP) or herniated disc.
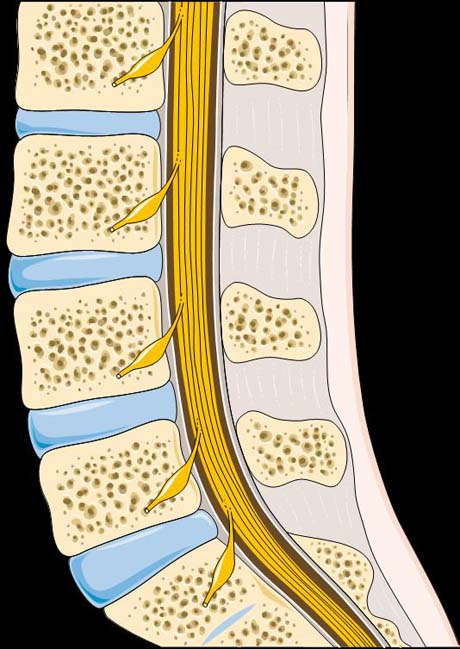
Νormal anatomy of the lumbur spine (profile)
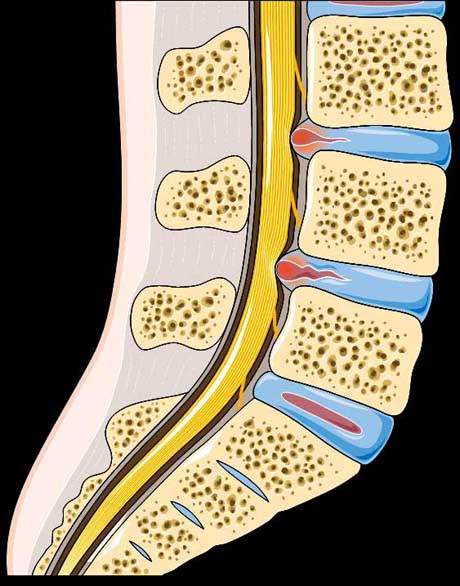
Discs herniations in two levels. The disc protrude in to the spinal canal (red spots)
HISTORY OF PATIENTS WITH DISC HERNIATION
Most people relate back and leg pain to a traumatic event, but close questioning sometimes reveals that patient have had intermittent episodes of back pain for months or years.
The pain may be brought on by heavy exertion, repetitive bending, twisting, or heavy lifting. Pain usually begins in the low back and radiates to the buttock area.
Radicular pain usually extends below the knee and follows the dermatome of the involved nerve root. When the patient have sustained a disc herniation, the pain usually increases with activities, especially with sitting position.
RISK FACTORS
- As normal consequence of aging, Intervertebral discs undergo degenerative changes, marked by dehydration of the nucleus pulposus. Progressive fibrillation, separation and tearing of annular fibers from prolonged axial and shear stress may result in a complete radial annular tear.
- Weight lifting with improper way. Using the back muscles to lift objects, instead of the legs
- Heavy Body weight. Exercise program create strong muscles around the lumbar spine, very important issue for healthy non herniated spine. The overweight body puts added stress on the Intervertebral discs.
- Prolonged sitting position with wrong way. The sitting position is the worse position for the low back. The proper support during sitting with McKenzie pillow is a good option.


