SURGICAL TREATMENT
Osteocondritis dissecans of the lateral femoral condyle in man 20 years old
Many new techniques for the treatment of articular cartilage damage exist with very good results.
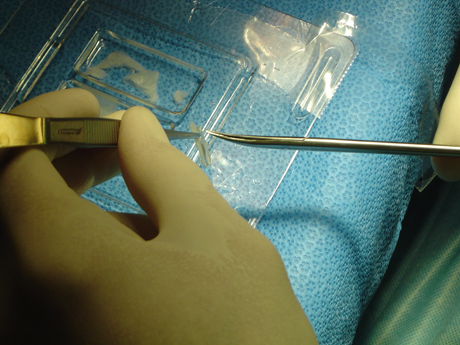
OSTEOCHONDRAL FRAGMENT STABILIZATION WITH SPECIAL PINS (ABSORBABLE)
The stabilization of osteochondral section shall be posted when the part is not separated completely from the anatomical position.
The procedure is done with arthroscopy of the knee where with the help of special tools placed by pin absorbable material so as to provide maximum stability.
MICROFRACTURE TECHNIQUE
Microfracture is indicated as first-line treatment for focal Outerbridge grade III and IV lesions under 3–4 cm2 in an otherwise nonarthritic knee in a symptomatic, active, and relatively young patient willing to respect the postoperative rehabilitation requirements.
Τhe microfracture techniques during knee arthroscopy. For older and low-demand patients, microfracture may be useful even in lesions larger than 3–4 cm2.
AMIC technique on knee chondral lesion - animated
Severe chondral patellar lesion in man 28 years old. AMIC technique
POSTOPERATIVE
Cold therapy is typically used for 1 to 7 days postoperatively.
Crutch-assisted touchdown weight-bearing ambulation (10% of body weight initially) is prescribed for 6 to 8 weeks, depending on the size of the lesion. For most patients, 6 to 8 weeks is adequate time to limit weight bearing. However, for patients with small lesions (<1 cm diameter), weight bearing may be initiated earlier.
Patients with lesions on the femoral condyles or tibial plateaus rarely use a brace during the initial postoperative period. However, we may prescribe an unloading type brace when the patient becomes more active and the postoperative swelling has resolved.
A CASE REPORT 1st
16-year-old Basketball athlete, suffers from knee joint pain left during the athletic activities initially but also during everyday activities.Clinical examination of the affected joint reproduce intense pain, especially during tibial torsion tests.
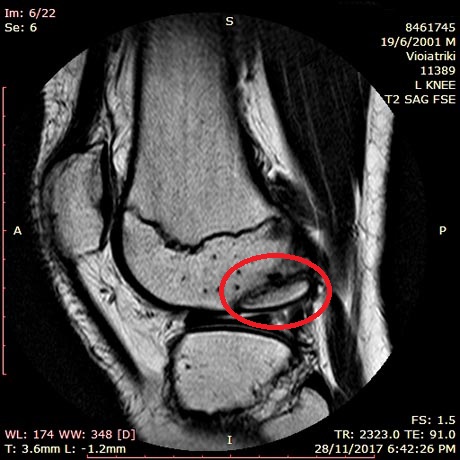
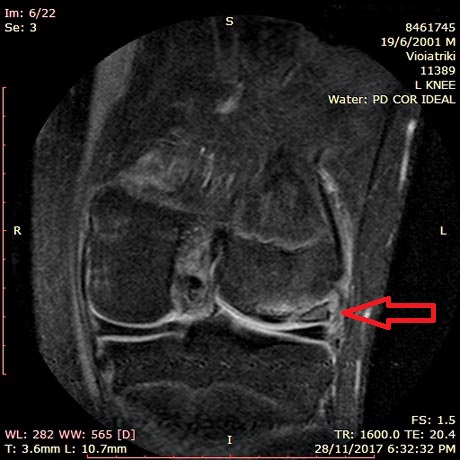
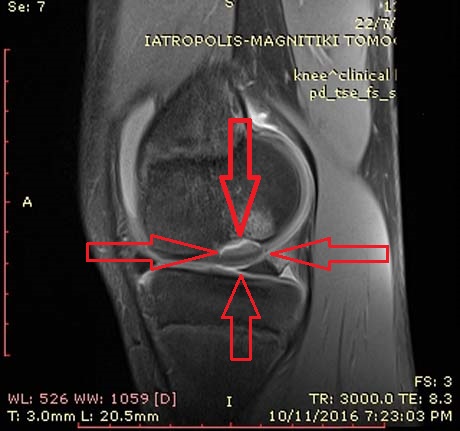
MRI of the left knee. Osteochondritis Dissecans of the lateral femoral condyle completely detached

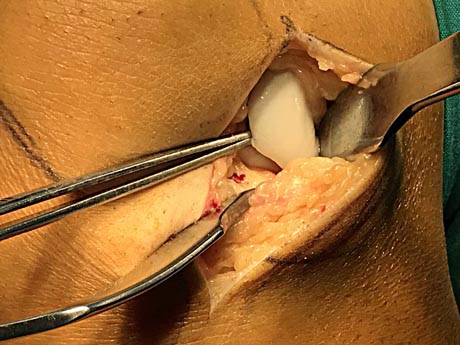
The damage of articular cartilage to the knee of the femoral condyle due to osteochondritis is completely detached from the surrounding healthy tissues and is removed.

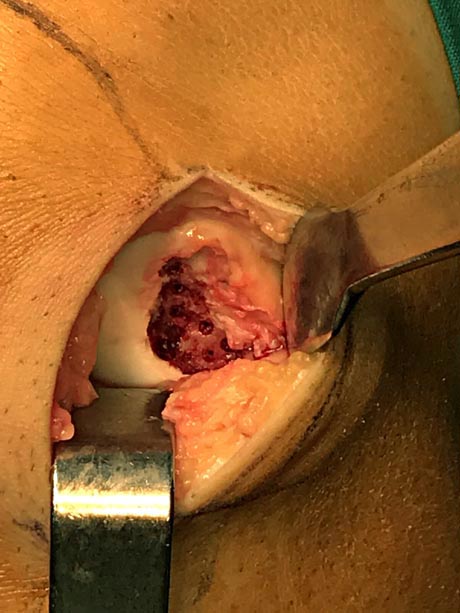
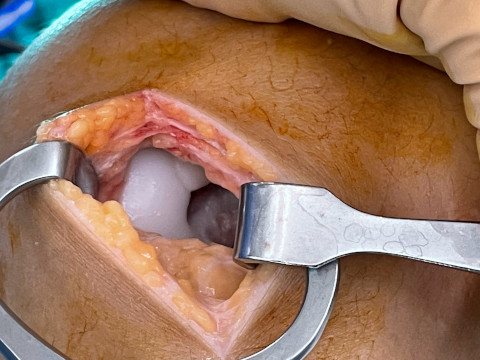
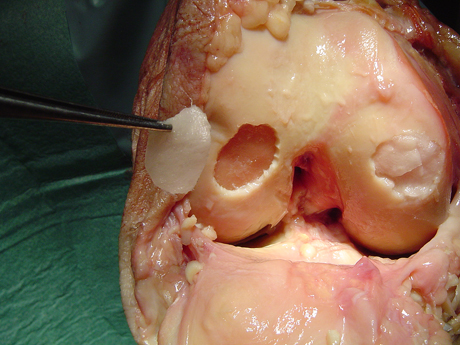
The buried osteochondral part is removed. The image shows the anatomical area after the part was removed


The necrotic part of the articular cartilage, which reaches a length of 2 cm

Nanofracture technique
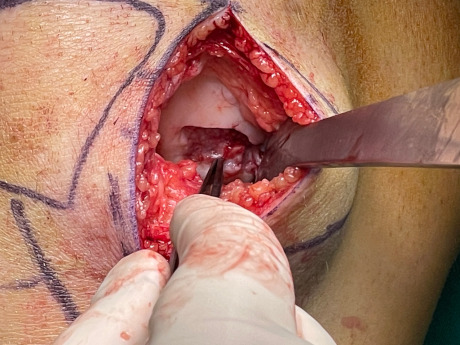
The nanofractures (Linvatec Conmed), in the crater of the damage

Apply the autografts to the base of the lession. The autografts come from the patient's pelvis.

Collagen membrane - AMIC technique above the grafts with special biologic glue

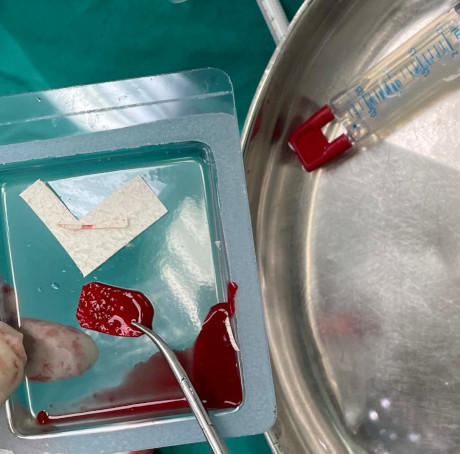
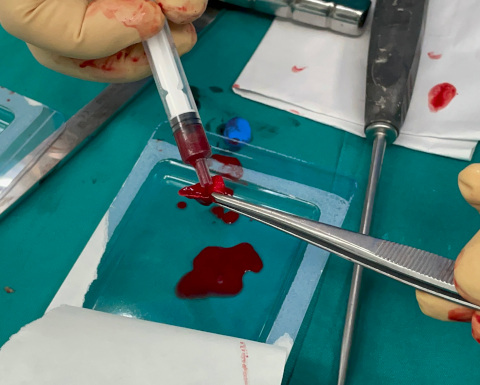
Taking bone marrow from the patient's pelvis (iliac bone). Advanced processing and isolation of autologous stem cell

Applying the stem cells to the surface of the collagen insert and stabilizing them with a bioadhesive agent

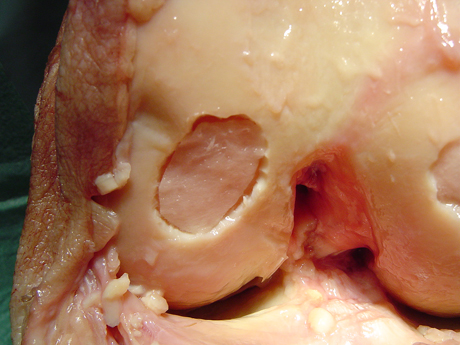
The space created by removal of the necrotic portion in the femoral condyle is covered by autologous grafts, collagen insert and stem cells.
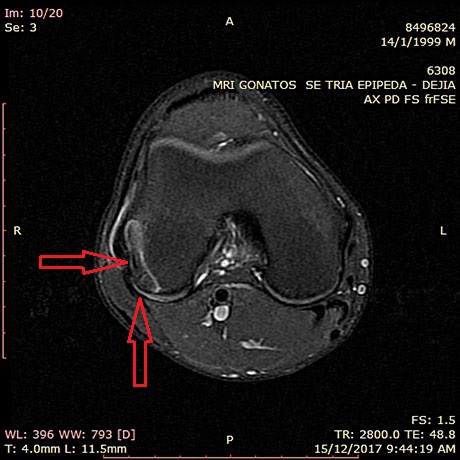
A cace report 2
A 23-year-old patient with a history of knee injury presents with severe pain months after the injury. MRI reveals damage to the articular cartilage in the femoral condyle -oost traumatic osteochondritis dissecans. The articular cartilage in the injured area had detached from its substrate and created a mechanical problem in the movement of the joint. The patient was treated with the AMIC method, ie the regenerative technique of the articular cartilage, in which stem cells from the patient's bone marrow (pelvic bone) are used, as well as a collagen membrane in combination with microfractures.

Traumatic damage to the articular cartilage - post traumatic osteochondritis dissecans. The articular cartilage is completely detached from its substrate.
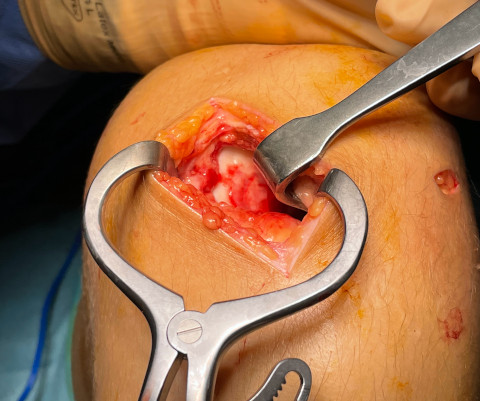
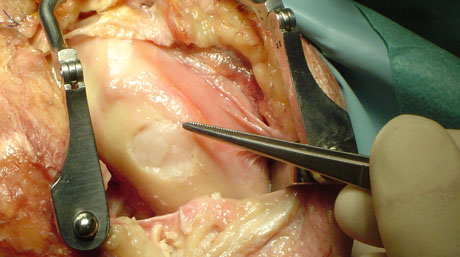
Removal of dead articular cartilage. The focus of the lesion on the femoral condyle in the knee.
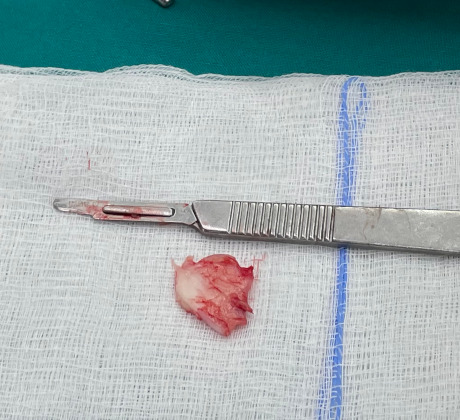
The part of the articular cartilage that detached after the joint injury.

Drilling at the base of the femoral condyle that aim to activate the healing processes of the articular cartilage.
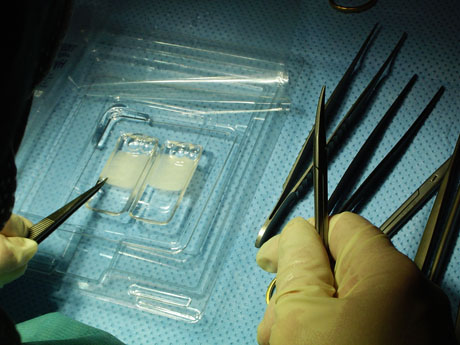
Collagen membrane enriched by the patient's stem cells which were obtained from the pelvic bones at the same time of the surgery.

Placement of bone grafts at the site of cartilage damage enriched in stem cells

Application of the collagen membrane

Final application of stem cells at the site of articular cartilage damage.
A case report 3
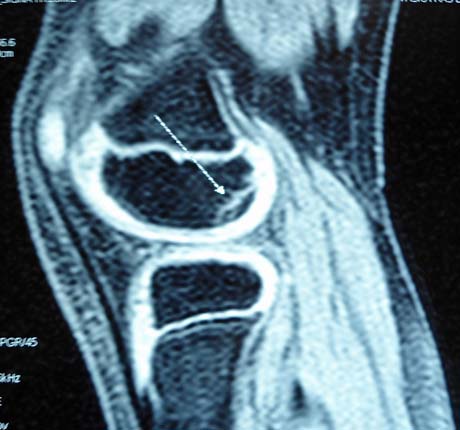
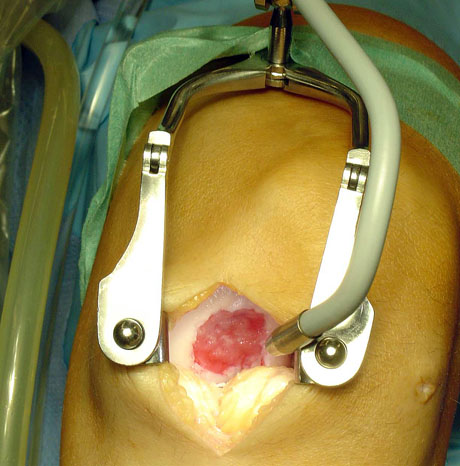
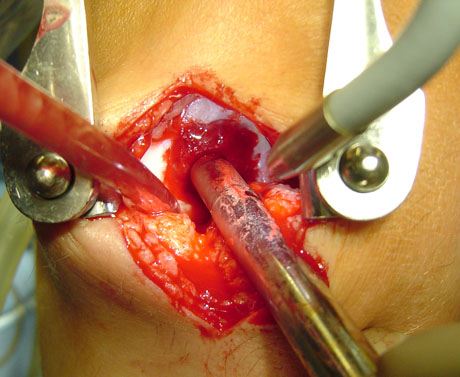
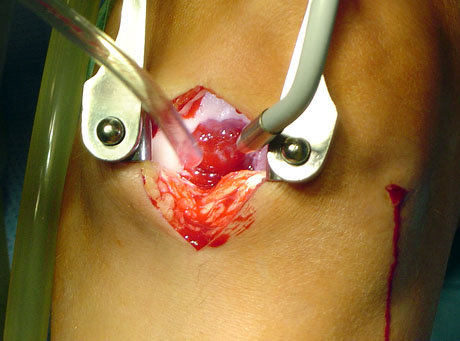
Male adolescent 15 years old with previous knee joint trauma history and osteochondral lesion of the medial femoral condyle
Osteochondral lesion of the medial femoral condyle due to osteochondritis Dissecans
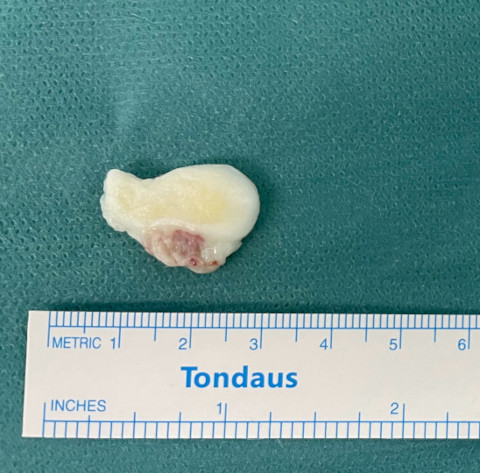
Osteochondral part as free foreign body in the knee joint that produce blockage of the joint.
Collagen membrane with autologous stem cells

Autologous cancelous bone from the pelvis

Autologous bone and collagen membrane - stem cells into the core of the lesion - final view.
AUTOLOGOUS CHONDROCYTE IMPLANTATION
Injuries to joint surfaces can result from acute high-impact or repetitive shear and torsional loads to the superficial zone of the articular cartilage architecture. The use of autologous chondrocyte implantation is promising and is associated with several potential long-term benefit.
Autologous chondrocyte implantation is ideally suited for symptomatic deep chondral lesion along the femoral condyle or trochlear region. High-demand patient between 15-55 years of age with excellent motivation and potential for compliance are the best candidates.
However autologous chondrocyte implantation is a viable option for a symptomatic patient with a lesion of >2 sq.cm but <12 sq.cm. and for a patient who continues to have pain after mosaicplasty or microfracture procedure. Bone involvement is not contraindication, but staged or concomitant autologous bone grafting should be undertaken when the bone involvement is deeper than 6-8 mm.
Autologous chondrocyte transplantation is not a treatment for osteoarthritis (general joint disease), gout, and rheumatoid arthritis or other systemic joint diseases.
Autologous chondrocyte are arthroscopicaly harvested from a less weight-bearing area, commercially extracted from the harvested cartilage (200-500mg), and multiplied in vitro (labor cell culture).
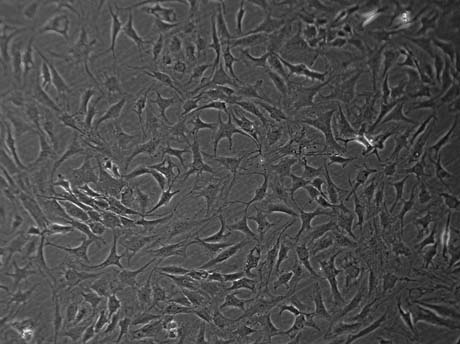
Chondrocyte cultivation in Bioengineer Lab
Elective reinplantation is performed 4-6 weeks after cartilage harnesting by debridement of the defect to an intact margin, carelully avoiding osseous bleeding from the bed of the defect.

The lesion area is already clear and ready to receveive the autologous chondrocyte.
Chondrocyte culture.
The surgeon cut the chondrocyte film like the shape of the chondral defect.
The autologous chondrocyte is ready to implant.
The autologous chondrocyte is transplanted. The chondral defect is covered.
Chondral defect due to trauma.
The autologous chondlal cell filling the defect.
The chondral defect covered by autologous chondrocyte atrhoscopically.
The arthroscopy procedure is finished. The knee movement is without any problem.
POSTOPERATIVE
Postoperatively protected weight-bearing are restricted for 6 weeks. The crutches is necessary for walking.
The physical therapy program started 2nd post-op day with passive movement (physical therapist or CPM machine) until 4th week. Therapy concentrates on quadriceps activation and isometric straight leg raises. After the 6th week the patient can walk without aid devices with full weight-bearing. Full weight bearing and full range of motion are achieved. Closed-chain exercises and functional training are started.
After 12th week Strengthening and functional training are progressed. Return to full activities is delayed for at least 8 months to protect the lesion as it matures.
Return to participation in pivoting sports is usually allowed by 12 months.